We Are Making Progress!
For the past three years Abilities In Motion has been leading the way in applying 3D printing technology to prosthetics. This video highlights our progress.

Stories of Inspiration and Hope
For the past three years Abilities In Motion has been leading the way in applying 3D printing technology to prosthetics. This video highlights our progress.
For many patients, this is one of the first questions that is asked when working with Abilities In Motion. Recently we spoke to Joy Lawson, an above knee amputee, about how she returned to driving after her amputation. For Joy, the primary motivator was the ability to have freedom and independence.
CLICK HERE TO SEE MORE DETAILED INSTRUCTIONS AND A LIST OF AREA DRIVING INSTRUCTORS/AUTHORIZED DEALERS
There are a variety of adaptive devices that can safely help individuals with disabilities operate a motor vehicle safely. Since Joy wears a prosthesis on her right side, her vehicle was modified with a left foot accelerator. For other amputees, the accelerator and brake can be regulated using hand controls. Because every situation is different, it’s important to consult a professional that can offer individualized options.
To comply with Ohio law and insurance regulations you will need to get a physician’s evaluation before returning to driving. Your physician may recommend that you receive specialized driving training and provide you a physical therapy prescription for this purpose. It’s important that you contact both your health and drivers insurance companies to see what benefits you may be entitled to asset you in this process. In general, Medicare does not provide benefits to provide financial resources for motor vehicle adaptive devices. A list of certified driving instructors can be found on our website (www.AbilitiesInMotion.com/Driving)
Once you have completed a clinical evaluation, and received a “Vehicle Modification and Adaptive Equipment Prescription for Driving and/or Transportation” from a Licensed Driver Instructor, you will need to take the prescription to a licensed dealership to have an adaptive equipment installed on your vehicle. Ohio American Bus & Accessories (800-582-7118, www.american-bus-inc.com) are authorized dealers in southwest Cincinnati.
Many individuals who have lower limb prosthetic devices can drive vehicles safely and effectively with a few modifications. This enables you to live your life more normally, relying less on others for transportation.
• Link to Request for Statement of Physician
• Many states have specific requirements for reporting conditions that affect your ability to drive.
• You must have a physician’s approval to return to driving.
• Speak with your doctor and therapist if you are considering a return to driving.
• You may need to have a clinical evaluation.
DRIVING SCHOOLS/RESOURCE CONTACTS
Trihealth.com
PHONE: 513-569-6777
Offers Driving Program by a licensed occupational therapist with behind-the-wheel evaluation. They require a physician’s prescription.
Bick’s Driving
PHONE: 513-251-2100
2-3 Hour Session
Need Driver License & Doctor Prescription. This is an out-of-pocket service.
Full Drivers Evaluation – Cost can range from $295-$350 (cost may change)
Behind the Wheel Evaluation – Cost can range from $150-$250 (cost may change)
Kettering Sports Medicine
PHONE: 937-395-3900
2-3 Hour Session. Need Driver License & Doctor Prescription
Full Drivers Evaluation – $150-$250 (cost may change)
Behind the Wheel – $150 (cost may change)
Takes Private Insurance – Does Not Take Medicare
• You may need a behind-the-wheel evaluation, which includes simple neighborhood driving and progresses (when safety allows) to highway driving.
• You may need specialty testing and training with car adaptations and equipment (i.e. lift, spinner knob, left foot accelerator, or hand controls).
• Your case manager can provide you with information on topics like how to obtain disability plates for your vehicle and arranging alternative methods of transportation
• Once you have completed a clinical evaluation, and received a “Vehicle Modification and Adaptive Equipment Prescription for Driving and/or Transportation” from a Licensed Driver Instructor, you will need to take the prescription to a licensed dealership to have an adaptive equipment installed on your vehicle.
Authorized Dealer in Cincinnati:
American Bus & Accessories
PHONE: 800-582-7118 / 513-821-3220
WEBSITE: www.american-bus-inc.com
123 CityCentre Drive
Cincinnati, OH 45216
FAX: 513-679-4424
(Estimated cost for left foot accelerator – $600-$800). Check with your individual insurance company for coverage.
•The Licensed Driver Instructor will also submit the recommendation for a drivers test to the Ohio Department of Public Safety Bureau of Motor Vehicles (BMV) who will invite you to take a Driving Test and Maneuverability Exam.
•Prior to taking a Driving / Maneuverability Exam, the BMV will first send a request for Statement of Physician form, (BMV 2310A) with an instruction letter regarding completing the form for you and your physician.
•After the BMV receives the “Request for Statement of Physician” form with an ok from the physician to operate a motor vehicle, the BMV will set up an appointment for the exam at a Driver License Exam Station.
*Information taken from Wellness Information & Tools for Health (WITH)
 Abilities In Motion’s Josh Sust has completed the training to become a certified peer visitor through the Amputee Coalition. The mission of the Amputee Coalition is “To reach out and empower people affected by limb loss to achieve their full potential through education, support and advocacy, and to promote limb loss prevention*”
Abilities In Motion’s Josh Sust has completed the training to become a certified peer visitor through the Amputee Coalition. The mission of the Amputee Coalition is “To reach out and empower people affected by limb loss to achieve their full potential through education, support and advocacy, and to promote limb loss prevention*”
 JOSH’S STORY: November 12, 2011 will forever be known as Corporal Joshua Sust’s Alive Day or the day he cheated death. On mounted patrol in Helmand Provence, Afghanistan, his unit encountered an Improvised Explosive Device (IED). Josh’s last memory that day was watching his helmet fly off his head, and he suffered major injuries to his left leg and arm.
JOSH’S STORY: November 12, 2011 will forever be known as Corporal Joshua Sust’s Alive Day or the day he cheated death. On mounted patrol in Helmand Provence, Afghanistan, his unit encountered an Improvised Explosive Device (IED). Josh’s last memory that day was watching his helmet fly off his head, and he suffered major injuries to his left leg and arm.
After three years of constant pain in his leg, Josh went through an elective procedure to amputate his badly injured leg. He had been inspired by the examples of his fellow Marines that are enjoying active lives with below knee amputations. Josh’s relationship with Abilities In Motion began when he was fitted for an IPOP (Removable Immediate Post Operative Cast) by Tom Walsh.
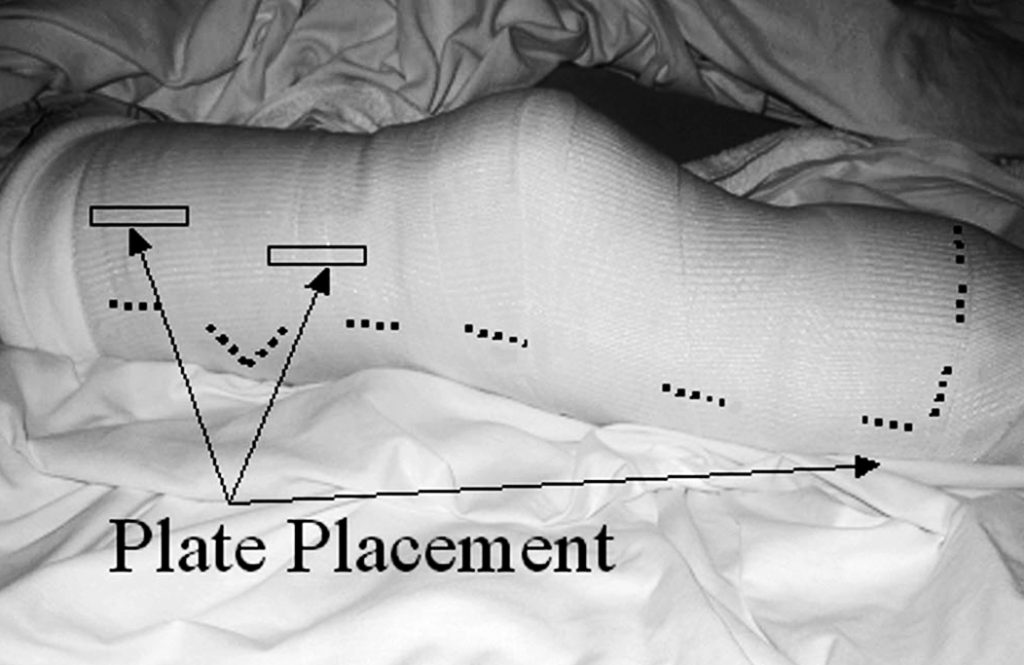
 This device was key to his recovery because it allows the patient to keep his/her leg straight and protects the incision site.
This device was key to his recovery because it allows the patient to keep his/her leg straight and protects the incision site.
On December 23, 2015, Josh received his new prosthesis, and he told the staff at Abilities In Motion, “It was the best Christmas present ever. Just being able to take that first step was an amazing feeling and accomplishment”. It was the start of a new life.
 Josh’s enthusiasm and zest for life is contagious. Because he wants to continue to pay it forward, it was a natural move to make Josh a valuable member of the Abilities In Motion team. “Josh is able to speak to patients with an empathy and understanding that only someone with his experiences can express,” says Tom Walsh. “He is able to coach and inspire patients to keep moving forward”.
Josh’s enthusiasm and zest for life is contagious. Because he wants to continue to pay it forward, it was a natural move to make Josh a valuable member of the Abilities In Motion team. “Josh is able to speak to patients with an empathy and understanding that only someone with his experiences can express,” says Tom Walsh. “He is able to coach and inspire patients to keep moving forward”.
*Source: Amputee Coalition
For Ron Davis, riding a motorcycle is not simply a hobby… it’s a way of life.
 In an instant everything changed. While on his bike another driver turned in front of him and he was involved in an accident that caused him to lose his left leg below the knee. Almost immediately, Ron was determined to ride again. “My goal at the beginning was to be able to be back on a motorcycle in less than a year,” said Ron.
In an instant everything changed. While on his bike another driver turned in front of him and he was involved in an accident that caused him to lose his left leg below the knee. Almost immediately, Ron was determined to ride again. “My goal at the beginning was to be able to be back on a motorcycle in less than a year,” said Ron.
When Ron was not getting the prosthetic solutions he needed from his provider, his doctor referred him to Abilities In Motion. The professionals at AIM were able to identify Ron’s particular needs and gave him components that he needed to ride again.
 “Abilities In Motion [has] been fabulous. You actually gave me a leg that I was looking for. I was looking for something that would actually pivot, the other place I was going to said I couldn’t have that. [AIM] made all the difference in the world, in my ability to walk from flat plain to going up hills, so I am thrilled with Abilities In Motion.”
“Abilities In Motion [has] been fabulous. You actually gave me a leg that I was looking for. I was looking for something that would actually pivot, the other place I was going to said I couldn’t have that. [AIM] made all the difference in the world, in my ability to walk from flat plain to going up hills, so I am thrilled with Abilities In Motion.”
Two days before the anniversary of his accident, Ron rode again. It was an emotional moment for Ron and his wife, as his motorcycle club gave him an ovation that he won’t soon forget.
Learn more about Ron by watching the video above.
Abilities In Motion has two locations in Cincinnati and is always seeking new and innovative ways to meet the needs of lower limb amputees. More information, including stories of other veterans can be found on their website at www.abilitiesinmotion.com.

Abilities In Motion has been leading the way with Immediate Postoperative Prosthesis (IPOP) procedures since 1995. This course of treatment has become preferred by doctors for individuals facing below the knee amputation. After the surgeon has completed their work, our staff creates a removable cast that protects the incision site, reduces swelling, decreases pain and allows the physicians to conduct regular inspections of the residual limb. In some cases, a temporary prosthesis can be attached to make it possible for some patients walk weeks after surgery.

Below are some quick facts about the procedure followed by an academic article that was published in the Journal of Prosthetics and Orthotics by Abilities In Motion’s own Tom Walsh. If you have any questions, please contact us live chat (below), by phone: (513) 245-0253 or by email.
Studies report that with the use of immediate post operative prosthesis and amputation level selection by xenon clearance, healing approached 100%.
Prior to the use of immediate post operative prosthesis, the primary healing rate ranged from 62% to 75%.
Many postoperative treatment modalities for the transtibial amputee are in current use. A simple gauze dressing is the treatment of choice for many surgeons. Another option is compression therapy using an ace bandage or stump shrinker. A more aggressive approach would include the use of a rigid dressing or an immediate postoperative prosthesis (IPOP).

The latter modality, although documented to offer the highest rate of healing, is possibly the least used because of many factors, including lack of familiarity with the treatment, a fear of placing a hard cast on a vascularly compromised limb, and the need to frequently monitor the wound. The traditional IPOP is a nonremovable cylinder cast. When the residual limb needs to be inspected, the cast is cut off using a cast saw. Another cast is then fabricated if the IPOP continues to be used. This article presents a removable IPOP, designed for the diabetic, peripheral vascular disease amputee, that specifically addresses the needs of the surgeon. In addition, the design permits a proactive clinical team approach, enhancing the treatment of the prosthetist and the physical therapist. (J Prosthet Orthot. 2003;15:158–161.)
Key Indexing Terms: Immediate postoperative prosthesis (IPOP), immediate postoperative prosthetic fitting (IPPF), amputation.

The concept of immediate postoperative prosthetic fittings (IPPF) is not new. In 1893, German surgeon von Bier reported fitting patients with temporary prostheses within days of amputation and allowed them to stand and walk. In 1961, Berlemont reported fitting patients with prostheses immediately after amputation surgery and initiating gait training in 1 to 2 days. In 1971, Burgess reported satisfactory results in 193 lower extremity amputations performed for peripheral arterial insufficiency; by 1978, he and his group had performed more than 1500 consecutive unselected amputations with the IPPF approach. Moore5 reports a considerable range of healing rates in literature before the use of immediate postoperative prosthesis (IPOP). The primary healing rate ranged from 62 to 75%. With the use of IPOP and amputation level selection by xenon clearance, healing approached 100%. In addition, Moore reports improved rehabilitation rates. Before the use of IPOP, the average rate of prosthetic rehabilitation in the geriatric amputee was 64%. With the use of the IPOP, a 100% prosthetic rehabilitation rate was achieved in unilateral amputees who had been ambulatory before amputation. More recently, in 1987, Wu and Krick reported the use and success of a removable rigid dressing. Although the primary purpose of their design was a non–weight-bearing rigid dressing, many of the principles are the same.
Despite these reported successes, use of the IPOP is not the standard of treatment for postoperative management of the amputee in the 21st century. Surgeons often cite the concern of skin breakdown and the need to inspect the surgical site for proper healing. The patient often lacks sensation and is unable to detect or report excessive pressure or friction caused by the cast. Often, the amputee is a geriatric patient with poor strength, and the potential for rehabilitation is unknown.
Still the overall purpose and results of the IPOP cannot be ignored. An IPOP may:
The purpose of this article is to present an easily and quickly fabricated IPOP designed to allow removal for wound inspection. By being removable, the design not only meets the needs of the surgeon but also benefits the entire rehabil- itation process. The prosthetist is allowed to make adjust- ments to accommodate for volume changes and to aid in limb shaping. The physical therapist is allowed to perform strengthening and range of motion exercises to the knee. The result is faster healing and a greater chance for successful rehabilitation.
Upon completion of the amputation, the surgeon applies a dressing of choice. It is important to note that the thickness of the dressing must be maintained throughout the process. Typically, the dressing does not extend proximal to the knee.
Figures 1 and 2 show the items needed in preparation for casting.


Typically, on postoperative day 1, the cast is bivalved and Velcro straps are applied.



A physical therapy evaluation is ordered and rehabilitation goals are set. Usually, standing and transfers are the initial goals, followed by hopping with a walker. If the patient is able to hop with the use of a walker or parallel bars, then the use of the pylon and prosthetic foot can be considered. The pylon and foot are attached, and 20 – 40 pounds of weight bearing is permitted. Zettl7 recommends 20 pounds of weight bearing and states that full weight bearing or weight bearing to tolerance can be counter-productive. A 20-pound weight- bearing limit has been found to be difficult to maintain during walking; therefore, the weight-bearing limit of 40 pounds has been permitted with good results. Typically, a scale is placed under the prosthetic foot and the patient is allowed to shift weight onto the IPOP and receive visual feedback as to when the weight bearing limit is achieved. The patient is then instructed to raise the contralateral limb while still maintaining the 20–40 pounds of weight bearing. When these goals are achieved, walking can begin (Figure 7),

In- struction on stairs and ramps follows. The pylon and foot are removed at the end of the physical therapy session. Once all goals are met, the amputee may use the pylon and foot for all activities of daily living. The patient is instructed on the application and removal of the pylon and foot, which can be
removed for sleeping or for activities such as getting into a vehicle. If the pylon and foot are worn during sitting for long periods, it is recommended that a footrest be used for sup- port.
Strengthening and range-of-motion exercises may be per- formed by removing the IPOP cast for short periods (Figure 8). The residual limb may have a tendency to swell when out of the cast and therefore should not be left out of the cast for more than 5–10 minutes. These exercises usually begin after the first wound inspection.

Postoperative management of the amputee should include measures to prevent falls. Barr et al. found that patients who have a primary diagnosis of lower limb amputation were five times more likely to fall than those who had a different primary diagnosis. A fall for the amputee can result in wound separation, often needing revision surgery. The IPOP provides a padded protective environment for wound healing. With the pylon and foot in place, the amputee functions with a more stable, bipedal gait.
For the surgeon to inspect the wound, the prosthetist does not have to be present. The surgeon simply unfastens the Velcro straps and removes the anterior shell of the cast. Instructing the patient to raise the extremity off of the bed by flexing at the hip, the posterior half of the cast can be removed. The Spandex cast socks are removed followed by the dressing. Make note that when reapplying the IPOP cast, the thickness of the gauze dressing must be maintained. The tendency is to apply a lighter dressing, which is counter-productive to maintaining distal compression. The fit of the IPOP cast must be continually monitored. By approximately postoperative day, the residual limb may experience a loss of edema and the IPOP cast becomes loose. An additional Spandex cast sock is applied to improve the fit of the cast and promote further shrinkage of the residual limb. Cast socks continue to be added throughout the time the cast is in place. A sock covering only the distal end of the limb is often used when distal shrinkage is not consistent with the thigh.
On the average, sutures are removed 21–28 days postop- eratively. After suture removal, a total contact below-the- knee prosthesis is fabricated to allow full weight bearing. If possible, the IPOP continues to be used until the total contact below the knee prosthesis is fitted, thereby maintaining func- tion and protection.
For the past 7 years, the removable IPOP has proven to be an effective adaptation to the original IPOP concept. The initial goal of the design was to meet the needs of the surgeon, which was to allow for easy wound inspection. The design later proved to be beneficial in the area of physical therapy to allow for strengthening and range of motion. In addition, the prosthetist is aided by the ability to adjust for residual limb volume loss and assist in limb shaping. All lead to a more cohesive clinical team approach with a better understanding of the challenges of postoperative management.
©American Academy of Orthotists and Prosthetists. Unauthorization reproduction of this article is prohibited.
1. Dederich R. Amputationen der unteren Extremitat. Operation- stechnik und prothetische Sofortversorgung. Stuttgart, Thieme, 1970.
2. Berlemont M. Notre experience de l’appareillage precoce des amputes des membres inferieurs aux establissments Helio- Marins de Berck. Ann Med Phys. 1961;4:4.
3. Berlemont M, Weber R, Willot JP. Ten years of experience with immediate application of prosthetic devices to amputees of the lower extremities on the operating table. Prosthet Orthot Int. 1969;3:8.
4. Burgess EM. Immediate postsurgical prosthetic fitting: A system of amputee management. Am J Phys Ther. 1971;51:139–143.
5. Moore WS. Below-knee amputation. In: Moore WS, Malone JM, eds. Lower Extremity Amputation. Philadelphia: WB Saunders Company; 1989:118–131.
6. Wu Y, Krick H. Removable Rigid Dressing for Below-knee Am- putees. Clin Prosthet Orthot. 1987;11:33–44.
7. Zettl, JH. Immediate Postoperative Prostheses and Temporary Prosthetics. In: Moore WS, Malone JM, eds Lower Extremity Amputation. Philadelphia: WB Saunders Company; 1989: 177–207.
8. Barr J, Brown P, Perry G. Risk factors associated with falls in the elderly rehabilitation client. Australas J Ageing. 1999;18:27–31.

Larry Robinson, 51 is a below knee amputee who had surgery in July of thisyear. Larry had elective surgery with the intent of having less pain and increased activity. He had a target of four weeks to be up and walking, and now believes he will be more active than he first thought. He was walking unassisted in just two weeks!
Larry experiences less phantom pain as time goes by and now has some discomfort but no pain. He quickly adapted to his prosthesis and has mastered sock fit with ease. He cites comfort as his favorite part of his prosthesis and would like to get more flexibility from his ankle to aid with his outdoor lifestyle of fishing and hunting. Larry also mentioned that he would like to have a prosthesis that lets his leg stay cooler.
 Walter Lickliter, 57 had a right below knee amputation in July of 2004. Walter also has a left partial foot amputation. His main goal before surgery was to improve his balance and begin the process of learning to walk again. Within two weeks of being fit with his prosthesis, Walter said “I am encouraged by my progress from wheel chair to walker. I have not had any pain since just after the surgery”. He learned quickly through experimentation how to use socks to obtain a correct fit and does not feel his prosthesis limits him. “I like the comfort of my prosthesis and just being able to walk again”.
Walter Lickliter, 57 had a right below knee amputation in July of 2004. Walter also has a left partial foot amputation. His main goal before surgery was to improve his balance and begin the process of learning to walk again. Within two weeks of being fit with his prosthesis, Walter said “I am encouraged by my progress from wheel chair to walker. I have not had any pain since just after the surgery”. He learned quickly through experimentation how to use socks to obtain a correct fit and does not feel his prosthesis limits him. “I like the comfort of my prosthesis and just being able to walk again”.

Tony Freeman, 50 is an above knee amputee who was fit with his first prosthesis in 1999. He said that after surgery the pain was “excruciating, but now I just have phantom pain that is annoying”. He expected to walk with a cane but after his initial fitting he thought he would have to work harder to be able to walk. Later during rehab, his target was to “just walk as normally as possible”. On the subject of learning the correct fit, “I just let my pain tell me what to do”.
“The thing I like most is my mobility, just being able to walk, although I would like to be able to go up stairs step over step”. Since rehab, Tony now cycles regularly and is able to run. Tony also said he would like a more flexible ankle, some rotation and a lighter prosthesis.
 Sarah Ammons underwent surgery for a below knee amputation in 2002. Sarah said “I expected to have less pain, as I have a great deal of phantom pain”. She did not expect to be walking unassisted immediately, “I expected a long rehab”. Although undergoing a second surgery earlier this year, she is walking without assistance.
Sarah Ammons underwent surgery for a below knee amputation in 2002. Sarah said “I expected to have less pain, as I have a great deal of phantom pain”. She did not expect to be walking unassisted immediately, “I expected a long rehab”. Although undergoing a second surgery earlier this year, she is walking without assistance.
“I am still learning to get the correct fit with socks” says Sarah. I would like to be able to walk longer distances without pain and to be able to go into the ocean. Also as a keen gardener, I would like more flexibility on uneven ground”. She also wanted it to be cooler and lighter.
 Sam Crosby has a left below knee and a right partial foot amputation. For Sam, a former college quarterback, rehab went very smoothly. “I just expected to be able to walk and I pretty much did. I knew I would be able to walk without crutches”. Sam reported that he never really had any pain and that learning sock fit was easy.
Sam Crosby has a left below knee and a right partial foot amputation. For Sam, a former college quarterback, rehab went very smoothly. “I just expected to be able to walk and I pretty much did. I knew I would be able to walk without crutches”. Sam reported that he never really had any pain and that learning sock fit was easy.
Sam is active, he plays golf and bowls. “I can pretty much do anything I want to”. “My favorite part of my prosthesis is the air pump that acts like a shock absorber”. Some of the improvements Sam wanted to see were a leg for swimming and a machine washable suspension sleeve.
 David Fischer became an above knee amputee just a few months ago in May. David says he wasn’t really sure what his expectations were prior to surgery as it happened so quickly. He said of his expectations upon receiving his prosthesis “I didn’t expect I would just get up and walk. I had a pretty good idea about the rehab process”. After initial fitting and physical therapy, David says he was more confident of being able to return to normal mobility. He has suffered from some phantom pain “but I’m managing well”.
David Fischer became an above knee amputee just a few months ago in May. David says he wasn’t really sure what his expectations were prior to surgery as it happened so quickly. He said of his expectations upon receiving his prosthesis “I didn’t expect I would just get up and walk. I had a pretty good idea about the rehab process”. After initial fitting and physical therapy, David says he was more confident of being able to return to normal mobility. He has suffered from some phantom pain “but I’m managing well”.
He quickly learned correct sock fit and gave some thought to the question of things he would like to be able to do. “I would like to be able to stand in the shower”. Like many of our panel, being able to walk is one of his favorite things about his prosthesis. As for improvements he would like to see, he agreed with several members of the panel in wanting to be able to get the leg wet and to have a lighter prosthetic foot.
A note from Tom:
Thanks to our esteemed panel for their time and thoughtful responses. Hopefully our panel’s shared experiences are relatable to most of you.
These comments will only help us to provide better service. We will also relay this information to our component manufacturers to address the needs of the people we serve.
Some of our panel had some questions for us, so we decided to do a little research.
Here are some statistics you may find interesting.